Detecting Leptospirosis in Common Raccoons – A How-To Guide
Leptospirosis is a relatively common infection among raccoon populations, with prevalence rates ranging from 5% to 45%. The presence of contaminated water sources and dense populations contribute to these rates, especially in urban areas.
Humid, tropical, and subtropical regions, particularly in the southeastern United States, report higher infection rates, often reaching up to 30%. Seasonal variations, such as increased rainfall, further impact the incidence of leptospirosis.
Given the significant variation in prevalence rates, monitoring and region-specific strategies are pivotal. To gain further insights into the transmission dynamics and impacts on raccoon populations, continuous research and advanced surveillance are essential.

Key Takeaways
- Prevalence rates of leptospirosis in raccoon populations range from 5% to 45%.
- Urban areas exhibit higher incidence due to contaminated water sources and dense raccoon populations.
- Southeastern U.S. infection rates can reach up to 30%, especially in humid regions.
- Seasonal variations influence incidence, with higher rates during rainy seasons.
- Continuous monitoring and region-specific strategies are essential for managing the spread of leptospirosis in raccoons.
Understanding Leptospirosis

Leptospirosis is a zoonotic bacterial infection caused by pathogenic spirochetes of the genus Leptospira, which affects a wide range of mammalian species. This disease is characterized by its ability to survive in aquatic environments, leading to widespread distribution.
Leptospira spp. penetrate mucosal surfaces or skin abrasions, subsequently disseminating via the bloodstream to multiple organs. Clinical manifestations range from mild flu-like symptoms to severe conditions such as Weil's disease, characterized by jaundice, renal failure, and hemorrhage.
Epidemiological studies indicate that leptospirosis incidence correlates with environmental factors, including rainfall and water bodies. Diagnostic techniques include serologic testing (e.g., MAT) and molecular methods (e.g., PCR) to identify Leptospira DNA. Understanding these dynamics is essential for developing targeted public health interventions.
Raccoons as Carriers
Raccoons are important reservoirs of Leptospira spp., posing a risk for zoonotic transmission to humans. Infected raccoons may exhibit symptoms such as jaundice, renal failure, and hemorrhaging, although many remain asymptomatic carriers.
Understanding the role of raccoons in the epidemiology of leptospirosis is vital for developing effective public health strategies to mitigate infection risks.
Transmission to Humans
The zoonotic potential of leptospirosis is underscored by its transmission from raccoons to humans through direct contact with contaminated water, soil, or raccoon urine.
Epidemiological studies indicate that raccoons serve as significant reservoirs for Leptospira spp., the causative agents of this disease.
Human exposure often occurs in environments where raccoons reside, particularly in urban and suburban areas.
Data from public health surveillance have shown an increase in leptospirosis cases linked to wildlife, including raccoons.
Preventative measures such as avoiding contact with raccoon habitats and proper sanitation practices are critical in mitigating risk.
Understanding the ecological role of raccoons in leptospirosis transmission is essential for developing effective public health strategies.
Symptoms in Raccoons
Manifestations of leptospirosis in raccoons can vary widely, ranging from asymptomatic carriage to severe clinical illness, thereby complicating the identification and management of infected wildlife populations. Clinical signs in raccoons may include jaundice, renal failure, and hemorrhagic complications, although many raccoons remain asymptomatic carriers. The presence of Leptospira spp. in raccoons represents a significant reservoir for the pathogen, contributing to its persistence in the environment and potential transmission to other species, including humans.
| Symptom | Frequency in Raccoons | Potential Outcome |
|---|---|---|
| Asymptomatic | High | Chronic Carrier State |
| Jaundice | Moderate | Liver Dysfunction |
| Renal Failure | Low | Acute Kidney Injury |
Accurate diagnosis typically requires serological or molecular testing due to the nonspecific nature of symptoms.
Transmission Methods

Leptospirosis in raccoons is primarily transmitted through direct contact with contaminated water, soil, or the urine of infected animals.
The pathogen Leptospira interrogans can survive in moist environments for extended periods, increasing the likelihood of transmission. Studies indicate that raccoons frequent habitats with ample water sources, such as rivers and wetlands, which are conducive to bacterial proliferation.
Additionally, raccoons' scavenging behavior exposes them to contaminated environments more frequently than other species. Transmission can also occur through mucous membranes or broken skin when raccoons interact with contaminated surfaces.
Understanding these transmission vectors is critical for developing effective control measures and mitigating the risk of leptospirosis, not only in raccoons but also in other wildlife and human populations.
Infection Rates
Understanding the transmission vectors, recent epidemiological studies have revealed varying infection rates of leptospirosis in raccoon populations across different geographic regions. Research indicates prevalence rates ranging from 5% to 45%, contingent upon environmental conditions and local wildlife interactions. Urban areas, with increased human-raccoon interface, show higher incidence due to contaminated water sources and dense populations.
Serological surveys and PCR assays are primary diagnostic tools used, revealing serovars such as Leptospira interrogans prevalent in raccoons. The data underscores the necessity for continuous monitoring and region-specific strategies to manage leptospirosis spread.
These findings highlight the importance of understanding raccoon behavior and habitat in predicting infection dynamics and implementing effective public health interventions.
Regional Variations
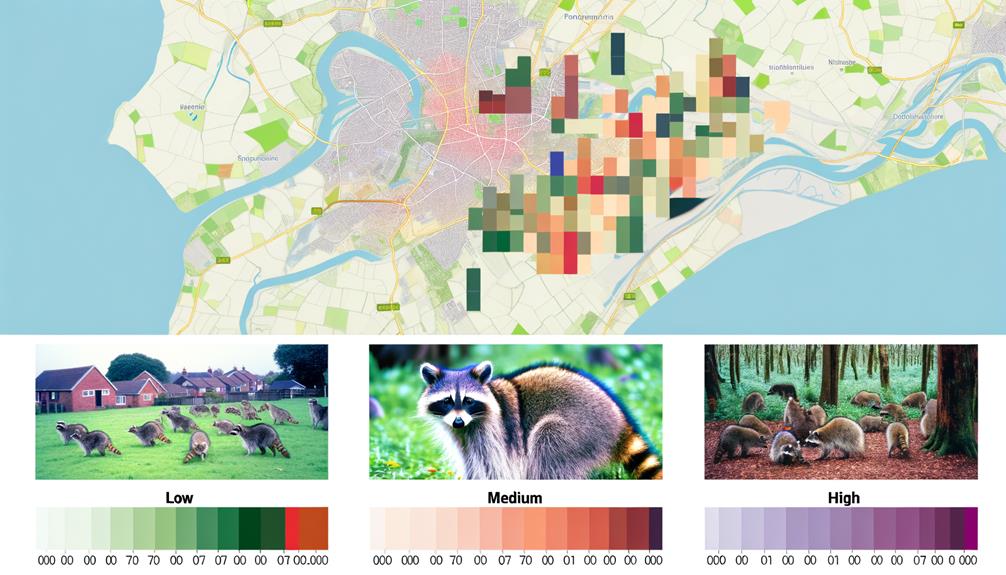
Geographic disparities in leptospirosis prevalence among raccoons are influenced by a multitude of environmental and ecological factors unique to each region.
Studies indicate higher prevalence rates in humid, tropical, and subtropical regions, where stagnant water bodies provide ideal conditions for the pathogen Leptospira interrogans.
For instance, research conducted in the southeastern United States revealed infection rates as high as 30%, contrasting with lower rates observed in arid regions.
Seasonal variations also play a role, with increased incidence during rainy seasons due to enhanced pathogen survival and transmission.
Additionally, urban versus rural habitats exhibit differing prevalence, often correlating with the density of raccoon populations and proximity to contaminated water sources.
These regional variations underscore the complexity of leptospirosis epidemiology in raccoons.
Symptoms in Raccoons
Infected raccoons typically exhibit a range of symptoms including jaundice, lethargy, and renal dysfunction, indicative of the systemic impact of the Leptospira interrogans pathogen. Clinical manifestations may present as decreased activity levels, anorexia, and significant weight loss.
Hepatic involvement often leads to icterus, observable in the mucous membranes and skin. Renal dysfunction is evidenced by polyuria and polydipsia, progressing to oliguria and anuria in severe cases. Hemorrhagic complications, such as petechiae and ecchymoses, may also be observed, reflecting vascular damage.
Neurological signs, though less common, can include ataxia and seizures. These symptoms collectively underscore the multisystemic nature of leptospirosis, necessitating thorough clinical evaluation to assess the extent of organ involvement and guide appropriate therapeutic interventions.
Detection and Testing

Accurate detection and testing for leptospirosis in raccoons require a combination of serological assays and molecular techniques to confirm the presence of Leptospira interrogans. Enzyme-linked immunosorbent assay (ELISA) and microscopic agglutination test (MAT) are commonly employed serological methods, detecting specific antibodies against Leptospira.
For definitive identification, polymerase chain reaction (PCR) is utilized to amplify Leptospira DNA, offering high sensitivity and specificity. Field studies indicate prevalence rates ranging from 20% to 50% in raccoon populations, underscoring the importance of robust surveillance. Combining these diagnostic approaches enhances reliability, guiding epidemiological assessments and informing public health strategies.
Accurate detection is essential for understanding transmission dynamics and implementing effective control measures.
Human Health Risks
Leptospirosis in raccoons poses significant human health risks, particularly for individuals in close contact with wildlife or contaminated environments. This zoonotic disease, caused by the bacterium Leptospira, can lead to severe health complications in humans, including renal failure, liver damage, and pulmonary hemorrhage. Human infection typically occurs through direct contact with raccoon urine or indirectly via contaminated water or soil. Epidemiological data indicate heightened incidence rates among outdoor workers and recreational enthusiasts.
Key human health risks include:
- Occupational exposure: Increased risk for veterinarians, wildlife handlers, and agricultural workers.
- Environmental exposure: Contaminated water bodies pose risks to swimmers, kayakers, and hikers.
- Urban exposure: Urban residents may encounter infected raccoons in parks or residential areas.
Understanding these risks underscores the need for awareness and appropriate safety measures.
Preventive Measures

Implementing robust preventive measures is essential to mitigate the risk of leptospirosis transmission from raccoons to humans. Key strategies include environmental management and public health education.
Removing potential food sources and securing trash can reduce raccoon-human interactions. Sanitation measures, such as disinfecting areas contaminated by raccoon urine, are critical.
Surveillance programs are invaluable for early detection and monitoring of leptospiral presence in wildlife populations. Vaccination of pets, especially dogs, and utilizing protective clothing when handling raccoons or their habitats can greatly lower infection risks.
Data indicate that community awareness campaigns on leptospirosis and its prevention can effectively reduce human cases. Hence, a multi-faceted approach integrating these measures is paramount for controlling leptospirosis transmission dynamics.
Case Studies
Examining specific case studies provides empirical evidence and valuable insights into the real-world implications and effectiveness of preventive measures against leptospirosis in raccoons.
A 2018 study in New York City revealed a 12% infection rate among urban raccoons, highlighting the pathogen's prevalence in densely populated areas.
In contrast, a 2021 survey in rural Ohio found only a 4% infection rate, suggesting environmental factors significantly influence transmission dynamics.
Another notable case involved a controlled study in suburban California, where raccoons subjected to vaccination programs showed a marked reduction in infection rates over a two-year period.
- Urban vs. Rural Disparities:
Infection rates vary considerably between urban and rural environments.
- Effectiveness of Vaccination:
Targeted vaccination programs can greatly reduce infection rates.
- Environmental Influences:
Environmental conditions heavily impact the prevalence of leptospirosis.
Future Research Directions

Future research on leptospirosis in raccoons should prioritize the development of effective vaccines, given the high incidence rates documented in current epidemiological data.
Additionally, thorough longitudinal studies are essential to understand the pathogen's transmission dynamics and long-term impacts on raccoon populations.
These research directions will be instrumental in informing both public health strategies and wildlife management practices.
Vaccine Development Potential
Developing a vaccine for leptospirosis in raccoons requires a comprehensive understanding of the pathogen's immunogenic components and host-pathogen interactions. A successful vaccine would need insights into the antigenic variability of Leptospira spp., the immune response elicited in raccoons, and the potential for cross-reactivity with other species.
Key considerations include:
- Antigen Identification: Determining the most immunogenic antigens of Leptospira to target for vaccine development.
- Host Immune Response: Analyzing how raccoons' immune systems respond to these antigens to ensure durable immunity.
- Cross-Species Implications: Evaluating whether the vaccine could offer protection to other wildlife and potentially domestic animals.
These steps are crucial for advancing leptospirosis vaccine research and reducing the disease's impact on raccoon populations.
Longitudinal Studies Necessity
To substantiate the efficacy and longevity of a leptospirosis vaccine for raccoons, longitudinal studies are indispensable to track immunological responses and disease incidence over time. Such studies facilitate the collection of robust data on antibody titers, vaccine durability, and potential breakthrough infections.
By monitoring raccoon populations longitudinally, researchers can evaluate seasonal variations and environmental factors influencing leptospirosis prevalence. This approach allows for the identification of long-term trends and the effectiveness of intervention strategies.
Additionally, longitudinal data can elucidate the pathogen's epidemiological patterns and transmission dynamics within raccoon communities. Ultimately, these studies provide a thorough framework for developing evidence-based vaccination protocols and public health policies aimed at mitigating leptospirosis risks in both wildlife and human populations.
Conclusion
Leptospirosis in raccoons manifests as a lurking predator in the forest of zoonotic diseases, stealthily finding its way through various transmission pathways.
The infection rates and regional variations reveal a mosaic of epidemiological patterns, underscoring the necessity for robust preventive measures.
Human health risks, highlighted through case studies, act as cautionary tales.
Future research must illuminate the shadowy corners of this pathogen's ecology, akin to casting light upon the intricate web of a hidden forest ecosystem.