Can You Get Rabies from Raccoon Poop?
Rabies transmission through raccoon feces is highly improbable. The rabies virus primarily spreads via the saliva of infected animals through bites or scratches.
While raccoons are notable carriers, the virus cannot survive long outside a host organism, making fecal transmission unlikely. However, raccoon feces can carry other pathogens, such as Baylisascaris procyonis, a parasitic roundworm.
Proper handling using personal protective equipment and disinfection is essential. Post-exposure prophylaxis and immediate medical consultation are recommended after any potential encounter with rabid animals.
For a thorough understanding of rabies transmission and prevention, further information is advisable.
Key Takeaways
- Rabies transmission through raccoon feces is highly improbable.
- The rabies virus cannot survive long outside a host organism.
- Rabies primarily spreads through direct contact with saliva or neural tissue.
- No documented evidence supports rabies transmission through feces.
- Proper handling of raccoon feces with PPE and disinfection is recommended.
Understanding Rabies
Rabies is a viral disease that mainly affects the central nervous system of mammals, leading to severe neurological symptoms and, if left untreated, death. The causative agent is the Lyssavirus, which attacks the brain and spinal cord.
Globally, rabies causes approximately 59,000 human fatalities annually, mainly in regions with inadequate healthcare infrastructure. The incubation period can vary from weeks to months, depending on factors such as the virus strain and the site of entry.
Early symptoms include fever, headache, and general weakness, progressing to acute neurological manifestations like agitation, hallucinations, and hydrophobia. Given its near 100% fatality rate once clinical symptoms appear, understanding rabies is critical for implementing effective public health measures and ensuring prompt post-exposure prophylaxis.
How Rabies Spreads
Transmission of the rabies virus primarily occurs through the saliva of an infected animal via bites or scratches. Rabies is a neurotropic virus that targets the central nervous system, leading to fatal encephalitis if untreated.
According to the Centers for Disease Control and Prevention (CDC), over 90% of reported rabies cases in the United States involve wildlife, with raccoons accounting for a significant portion. In rare instances, rabies can be transmitted via mucous membranes or open wounds exposed to infected saliva.
Despite its association with saliva, there is no documented evidence supporting transmission through feces. This data underscores the critical need for immediate medical attention following potential exposure, such as animal bites, to mitigate the risk of rabies infection.
Raccoon Behavior and Rabies
Understanding raccoon behavior is essential for comprehending their role in the epidemiology of rabies. Raccoons are nocturnal mammals known for their adaptability to urban environments, increasing the likelihood of human and pet encounters. Rabies transmission in raccoons is primarily through saliva via bites.
Key behavioral traits of raccoons that elevate rabies risk include:
- Foraging Habits: Raccoons often scavenge in residential areas, leading to frequent contact with humans and domestic animals.
- Territoriality: Infected raccoons may exhibit aggressive behavior, heightening the risk of bite incidents.
- Social Interaction: Higher interaction rates among raccoons facilitate the spread of rabies within their populations.
Can Feces Transmit Rabies?
Evidence indicates that rabies transmission through feces is highly improbable due to the virus's inability to survive long outside a host organism. Rabies virus is highly sensitive to environmental conditions, rapidly losing infectivity once exposed to air and sunlight.
Studies demonstrate that rabies primarily spreads through direct contact with saliva or neural tissue from an infected animal, typically via bites. The Centers for Disease Control and Prevention (CDC) confirms that rabies virus does not persist in feces, making transmission via this route exceptionally rare.
Thorough wildlife disease surveillance further supports this finding, showing no documented cases of rabies transmission through fecal matter. As a result, the risk of contracting rabies from raccoon feces remains negligible, ensuring public safety when managed appropriately.
Common Myths About Rabies
Numerous misconceptions persist about rabies, often leading to unnecessary fear and misunderstanding about the disease. Here are three common myths:
- Rabies is always fatal: While rabies is indeed serious, modern medical interventions, such as post-exposure prophylaxis (PEP), are highly effective when administered promptly.
- All animals can transmit rabies: Not all animals are reservoirs for the rabies virus. Primarily, it is transmitted by certain mammals like bats, raccoons, skunks, and foxes.
- You can get rabies from touching animal feces: Rabies spreads through saliva and neural tissue, not feces. The risk of transmission via feces is virtually nonexistent.
Understanding these facts helps mitigate undue fear and promotes informed decision-making in potential rabies exposure scenarios.
Other Risks of Raccoon Feces
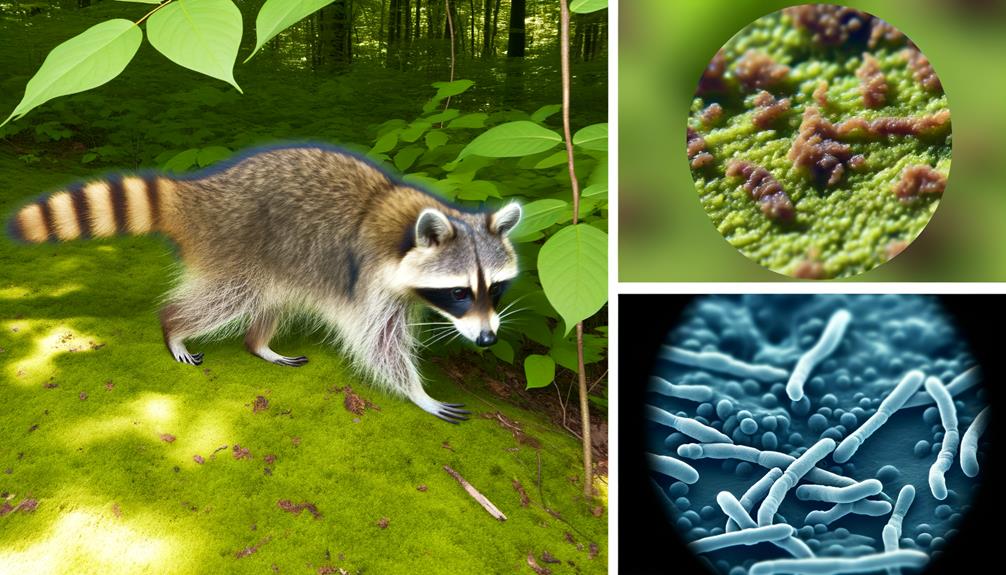
Raccoon feces present various health risks beyond rabies, including the transmission of parasites such as Baylisascaris procyonis, a roundworm that can cause severe neurological damage in humans.
Additionally, bacterial infections like Salmonella and Leptospira pose significant threats.
Environmental contamination from raccoon feces can also lead to widespread public health concerns, necessitating careful management and sanitation practices.
Parasites in Raccoon Feces
How significant are the risks posed by parasites found in raccoon feces to human health?
The presence of parasites in raccoon feces is an essential public health concern, as they can lead to severe infections.
Notable parasites include:
- Baylisascaris procyonis: This raccoon roundworm can cause serious neurological damage in humans if ingested.
- Giardia: This protozoan can lead to gastrointestinal issues such as diarrhea, cramps, and nausea.
- Cryptosporidium: Another protozoan, it is known for causing cryptosporidiosis, which results in severe diarrheal illness.
Data indicates that these parasites can be particularly risky to children, elderly individuals, and those with compromised immune systems.
Hence, proper hygiene and preventive measures are necessary to mitigate these risks effectively.
Bacterial Infections Risk
Exposure to raccoon feces can also pose significant risks due to the presence of harmful bacteria such as Salmonella and Leptospira. Studies indicate that approximately 5-10% of raccoon fecal samples test positive for Salmonella, a bacterium responsible for severe gastrointestinal infections.
Leptospira, another pathogenic bacterium found in raccoon feces, can cause Leptospirosis, a disease with symptoms ranging from mild flu-like conditions to severe kidney or liver damage. Infections from these bacteria can be particularly harmful to vulnerable populations, including children and those with compromised immune systems.
Proper hygiene practices, including wearing gloves and thoroughly washing hands after handling raccoon feces, are essential in mitigating these bacterial infection risks and ensuring community health and safety.
Environmental Contamination Concerns
In addition to bacteria-related health risks, raccoon feces can greatly contribute to environmental contamination, introducing hazardous pathogens and parasites into soil and water sources. This poses significant risks to both public health and environmental integrity.
Remarkable concerns include:
- Baylisascaris procyonis: This roundworm can cause severe neurological damage in humans and animals. Contaminated soil or water can facilitate its spread.
- Leptospirosis: This bacterial infection can enter water systems, posing a threat to humans through contact or ingestion, potentially leading to severe health complications.
- Giardia: This protozoan parasite can contaminate water sources, causing gastrointestinal illness in humans and animals.
Understanding these risks is essential for implementing effective mitigation strategies to protect public health and maintain environmental safety.
Symptoms of Rabies
Rabies symptoms typically begin with nonspecific signs such as fever, headache, and general malaise before progressing to more severe neurological manifestations. The disease can advance rapidly, leading to acute neurological symptoms such as confusion, agitation, and hallucinations. Paralysis and coma often follow, culminating in fatality if untreated.
| Symptom Stage | Initial Symptoms | Advanced Symptoms |
|---|---|---|
| Early | Fever | Confusion |
| Early | Headache | Agitation |
| Early | General Malaise | Hallucinations |
| Late | Paralysis | Coma |
Recognizing these symptoms early is vital for effective intervention. The initial phase might be mistaken for less severe illnesses, but the progression to neurological impairment underscores the need for immediate medical attention. Understanding this symptomatology can aid medical professionals and the general public in timely diagnosis and treatment.
Safe Handling of Raccoon Feces
While rabies transmission through raccoon feces is highly unlikely, proper handling and disposal are necessary to prevent other zoonotic diseases.
Raccoon feces can harbor pathogens such as Baylisascaris procyonis, a parasitic roundworm. To mitigate risk, consider the following safety measures:
- Personal Protective Equipment (PPE): Wear disposable gloves, masks, and eye protection to minimize direct contact with feces and inhalation of airborne particles.
- Disinfection: Use a bleach solution (one part bleach to nine parts water) to disinfect contaminated areas thoroughly.
- Safe Disposal: Double-bag feces and contaminated materials in heavy-duty plastic bags, and dispose of them in accordance with local waste management regulations.
Employ these measures to safeguard public health and prevent the spread of zoonotic diseases.
Preventing Rabies Exposure
To effectively minimize the risk of rabies exposure, implementing thorough vaccination programs for pets and humans in high-risk areas is crucial. Data indicates that vaccinating pets reduces human rabies cases by up to 99%.
Regularly scheduled vaccinations for dogs, cats, and ferrets should comply with local regulations. Additionally, public health initiatives should focus on raising awareness about rabies transmission, emphasizing the crucial role of avoiding contact with wild animals such as raccoons.
For communities in endemic regions, post-exposure prophylaxis (PEP) availability is essential. Surveillance systems must be established to monitor and report rabies cases promptly. These measures, combined with responsible pet ownership and community education, form a robust defense against rabies exposure.
When to Seek Medical Help
Recognizing the importance of seeking medical help promptly after potential rabies exposure is crucial for effective treatment and prevention. Rabies is nearly always fatal once symptoms appear, making timely intervention essential.
If you suspect exposure, follow these steps:
- Immediate Cleaning: Wash the affected area thoroughly with soap and water for at least 15 minutes to reduce viral load.
- Medical Consultation: Visit a healthcare provider immediately. They will assess the risk and may recommend post-exposure prophylaxis (PEP), which includes a series of rabies vaccinations.
- Follow-up Care: Adhere strictly to the vaccination schedule and attend all follow-up appointments to guarantee complete protection.
Prompt action can prevent the onset of rabies, safeguarding both individuals and the community.
Conclusion
While rabies is a serious zoonotic disease, transmission through raccoon feces is very unlikely. Rabies is primarily spread through bites or saliva from an infected animal. An interesting statistic is that over 90% of rabies cases in the United States occur in wildlife, with raccoons being a significant reservoir.
Understanding transmission routes and proper handling of animal waste are essential in preventing exposure. Immediate medical attention is necessary if potential rabies exposure occurs.